What’s the Difference Between SSRIs and SNRIs?
If you’ve been prescribed antidepressants or are researching treatment options for depression or anxiety, you might wonder: What’s the difference between SSRIs and SNRIs? Understanding these two common medication classes can help you make informed decisions about your mental health care.
At Dignity Brain Health, we specialize in tele-psychiatry medication management for adults throughout Massachusetts, including Boston neighborhoods like Brookline, Cambridge, Newton, Somerville, and Back Bay, as well as New Hampshire and Florida. Whether you’re searching for psychiatric medication near me, a psychiatrist online, or want guidance on antidepressants, this article explains the key differences and how each medication works.
What Are SSRIs?
SSRIs, or Selective Serotonin Reuptake Inhibitors, are the most commonly prescribed antidepressants.
How SSRIs Work
SSRIs increase the availability of serotonin, a brain chemical (neurotransmitter) linked to mood, by blocking its reabsorption (reuptake) into nerve cells.
This increased serotonin helps improve mood and reduce anxiety.
Common SSRIs
Fluoxetine (Prozac)
Sertraline (Zoloft)
Escitalopram (Lexapro)
Paroxetine (Paxil)
Citalopram (Celexa)
What Are SNRIs?
SNRIs, or Serotonin-Norepinephrine Reuptake Inhibitors, are another class of antidepressants that affect two neurotransmitters.
How SNRIs Work
SNRIs block the reuptake of both serotonin and norepinephrine, increasing their levels in the brain.
Norepinephrine plays a role in alertness, energy, and stress response.
Common SNRIs
Venlafaxine (Effexor)
Duloxetine (Cymbalta)
Desvenlafaxine (Pristiq)
Levomilnacipran (Fetzima)
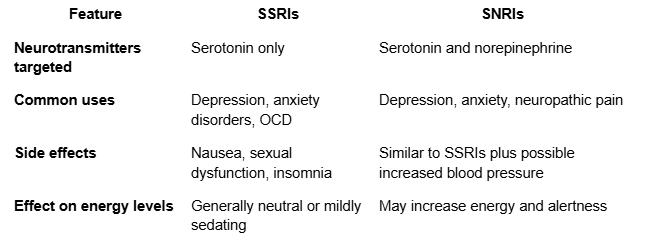
Key Differences Between SSRIs and SNRIs
When Might a Provider Choose an SNRI Over an SSRI?
If a patient does not respond well to SSRIs
Presence of chronic pain or fibromyalgia (SNRIs like duloxetine can help)
When increased energy or alertness is needed
Are SSRIs or SNRIs More Effective?
Both SSRIs and SNRIs are effective for depression and anxiety, but individual responses vary. Your provider will tailor treatment based on your symptoms, medical history, and side effect profile (Cipriani et al., 2018).
Telehealth Psychiatric Medication Management at Dignity Brain Health
We provide:
Comprehensive psychiatric evaluations via secure video
Expert guidance on choosing the right antidepressant class
Ongoing medication monitoring and dose adjustments
Genetic testing to help predict medication response (Learn More)
Serving adults in Boston metro areas including Brookline, Cambridge, Newton, Somerville, and Back Bay, with flexible scheduling and easy online booking.
Common Patient Questions
Can I switch from an SSRI to an SNRI?
Yes, with your provider’s guidance, switching medications is common if needed.
Do SSRIs and SNRIs have withdrawal symptoms?
Both can cause discontinuation symptoms if stopped abruptly; gradual tapering is advised.
How long do these medications take to work?
Typically 4 to 6 weeks to notice significant improvement.
Are there any serious risks?
Most side effects are manageable; rare risks include increased blood pressure with some SNRIs.
Local Mental Health Resources in Massachusetts
NAMI Massachusetts: Education and support https://www.namimass.org
Massachusetts Department of Mental Health: Public mental health programs
Harvard Medical School, Mass General, McLean Hospital: Leading research and care centers
Why Choose Dignity Brain Health?
Licensed psychiatrists and psychiatric nurse practitioners specializing in medication management
Telehealth care available statewide with a focus on Boston and surrounding neighborhoods
Personalized, evidence-based treatment plans
Convenient online appointment booking and follow-up care
Genetic testing for personalized medication decisions (Learn More)
Meet our expert team on our About Us page.
Take the Next Step: Book Your Telehealth Appointment Today
If you’re considering antidepressants and want guidance on SSRIs vs. SNRIs, get expert care from home with Dignity Brain Health.
👉 Start your your online psychiatric medication consultation process now
References
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., ... & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. The Lancet, 391(10128), 1357-1366. https://doi.org/10.1016/S0140-6736(17)32802-7
Stahl, S. M. (2013). Stahl's Essential Psychopharmacology: Neuroscientific Basis and Practical Applications (4th ed.). Cambridge University Press.
Gelenberg, A. J., Freeman, M. P., Markowitz, J. C., Rosenbaum, J. F., Thase, M. E., Trivedi, M. H., & Van Rhoads, R. S. (2010). Practice guideline for the treatment of patients with major depressive disorder (3rd ed.). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890423387
Fava, M. (2000). Diagnosis and definition of treatment-resistant depression. Biological Psychiatry, 48(8), 649-659. https://doi.org/10.1016/S0006-3223(00)00994-3